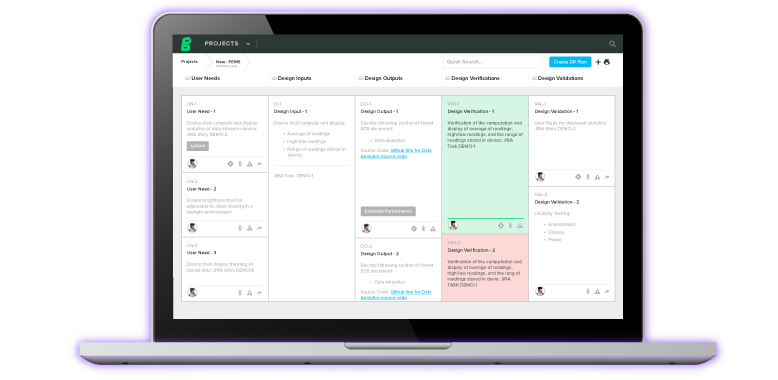
When you first start designing and developing a new medical device, you’re investing a lot of time, whether that’s in studying design controls, design inputs and outputs, or measuring and mitigating risk.
So, when it comes time to create the labeling for the device, it’s tempting to write these steps off and assume it’s going to be easy. However, the opposite is true. Not only does medical device labeling have to adhere to strict regulations in markets around the world, it also covers far more ground than you’d expect.
Let’s dive into three of the most common misconceptions about medical device labeling.
Misconception #1: Medical device labeling is just the label on the device
The purpose of medical device labeling is to inform patients and caregivers about the proper use, risks, and benefits of a given device in language they can understand.
To do so, you need to provide end users with adequate information about how the device works, its care and maintenance, and how its use fits into a care regimen. Without thorough labeling to prevent misuse, a manufacturer’s device could put its users at risk.
That’s why regulatory bodies like FDA and the International Organization of Standardization (ISO) take a broad approach when it comes to what they consider to be medical device labeling.
In 21 CFR Part 801, FDA describes labeling as:
All labels and other written, printed, or graphic matter upon any article or any of its containers or wrappers, or accompanying such article at any time while a device is held for sale after shipment or delivery for shipment in interstate commerce. The term 'accompanying' is interpreted liberally to mean more than physical association with the product. It extends to posters, tags, pamphlets, circulars, booklets, brochures, instruction books, direction sheets, fillers, etc.
This section tells us that labeling does not end with what’s stamped on the device; it extends to any messaging on the interface, point-of-sale displays, packaging, or documents included with the purchase. The definition also extends to claims made in advertisements, whether those are communicated in writing, or orally, such as in a radio or video advertisement.
ISO 13485, the international standard for medical device quality management systems, defines labeling as:
The label, instructions for use, and any other information that is related to identification, technical description, intended purpose and proper use of the medical device.
Here, we see that labeling requirements apply not just to how or where information is communicated, but also the content of the included descriptions. This is made clear by the great level of importance ISO places on the instructions for use (IFU).
The IFU of a device must be thorough and informed by an accurate understanding of who the users are, their strengths and limitations, and different ways they might interact with the product. You can develop that understanding through a combination of techniques, such as focus groups, interviews, field research, contextual inquiries, and literature reviews.
Whatever technique you use, though, it’s abundantly clear that you cannot leave labeling until the very end of the project. Medical device labeling requires intentionality, not simply copying what the other guys did.
Which brings us to the next misconception.
Misconception #2: Medical device labeling for 510(k) submissions can be the same as its predicate device
510(k) submissions hinge on demonstrating substantial equivalence through a comparison to a chosen predicate device. When you’re designing your device labeling, you can start with the predicate device label. It will give you a good starting point for what warnings and cautions you might need to include.
But you can’t stop there.
Your labeling is part of your design outputs and needs to be treated as such.
You also need to make sure you’re connecting your label to your risk management. If you’ve identified hazardous situations or harms that aren’t mentioned on the predicate label, you need to make sure you consider including them on yours.
In some cases, the predicate device was created years before your device and new information about hazardous situations and harms may be available now that wasn’t before. As for the rest of the labeling, specifically the IFU, don’t assume that you can just swap out the information on how to use the predicate device with how to use yours.
There are two general categories of information that may be included in medical device labeling:
-
Risk/benefit information, which is the information people need to decide to use a device or have it used on them. This information also allows the users to become aware of potential problems with the device.
-
Instructions for Use, which are the procedural steps to follow in setting up, using, cleaning, troubleshooting, and storing a device. This information constitutes the “how to” for the device.
Both of these areas refer back to the intended use of a device. The same can be said for substantial equivalence and how a new proposed product relates back to a predicate device.
There needs to be a clear understanding and communication of both the predicate and the new device. Without that being adequately explained, the clearance of a 510(k) submission could be delayed or rejected.
Misconception #3: The address on the medical device labeling is where the device is made
In today’s world, more and more medical devices are being made by contract manufacturers or in a different corporate location. With all of these locations involved, which one goes on the labeling? It actually depends on where you’re selling your device.
Under 21 CFR Part 801.1, the FDA requires that the label “shall specify conspicuously the name and place of business of the manufacturer, packer, or distributor.” And that if a “device is not manufactured by the person whose name appears on the label, the name shall be qualified by a phrase that reveals the connection such person has with such device; such as, ‘Manufactured for ___’, ‘Distributed by _____’, or any other wording that expresses the facts.”
This means that you can put your company’s address on the label, not the contract manufacturer’s, as long as you clearly state it’s manufactured for you. It is another example of the importance of using a risk-based approach for your medical device, as it protects both the user’s safety and your own liability.
A similar aspect of risk management in medical device labeling can be found in the regulations for devices that are repurposed by an approved distributor. Off-label use for devices may potentially cause unforeseen or undesired effects on patients and users. What if a repurposed device is resold without its original labeling? How can manufacturers protect themselves from liability, especially if their address is printed directly on the device?
FDA addresses this in 21 CFR 801.4, stating:
The intended use(s) of an article may change after it has been introduced into interstate commerce by its manufacturer.
If, for example, a packer, distributor, or seller intends an article for different uses than those intended by the person from whom he received the devices, such packer, distributor, or seller is required to supply adequate labeling in accordance with the new intended uses.”
However, if a manufacturer knows, or has knowledge of facts that would give him notice that a device introduced into interstate commerce by him is to be used for conditions, purposes, or uses other than the ones for which he offers it, he is required to provide adequate labeling for such a device which accords with such other uses to which the article is to be put.
By viewing medical device labeling as an extension of risk management, manufacturers are able to return to the very reason a medical device was made: to improve the quality of people’s lives.
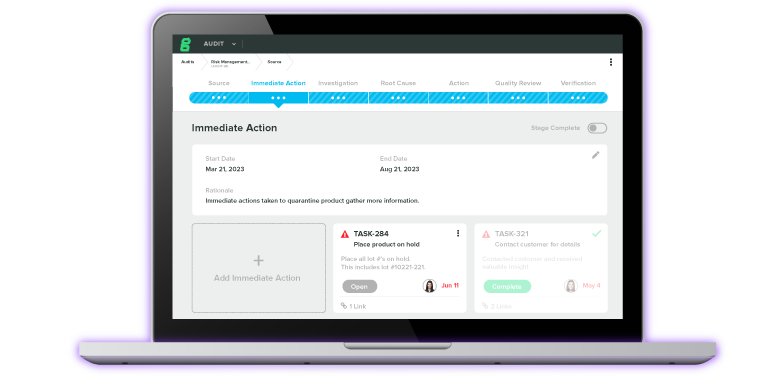
Connect your medical device labeling to design and risk controls with the right QMS
Medical device labeling shouldn’t be treated as an afterthought, but rather as another vital component of designing and manufacturing quality products. In order to do this, you’ll need to integrate risk management throughout the product development lifecycle.
By integrating the risk management process into your entire QMS, you can fix issues that expose you to risk when it’s less expensive and time-consuming to do so.
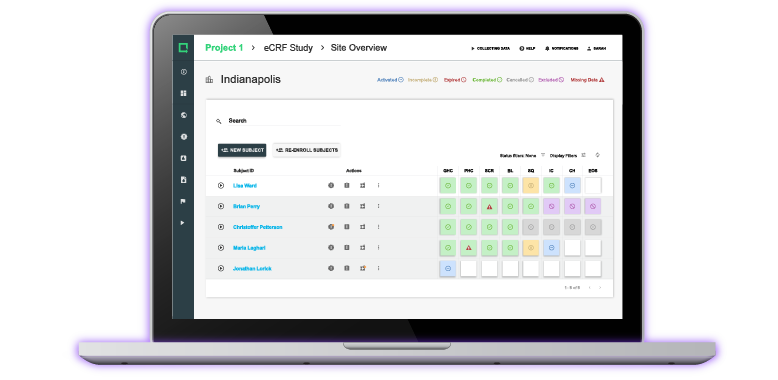
That’s exactly what Greenlight Guru provides to your team. As the only turnkey QMS solution built specifically for the medical device industry, you can easily link and connect design controls and documents as risk control measures to mitigate and reduce risks throughout the entire product lifecycle.
Interested in learning more? Contact us today for your free personalized demo!
Etienne Nichols is a Medical Device Guru and Mechanical Engineer who loves learning and teaching how systems work together. He has both manufacturing and product development experience, even aiding in the development of combination drug-delivery devices, from startup to Fortune 500 companies and holds a Project...
Related Posts
When Design Inputs Go Wrong + Design Your Label Like You Design Your Device
Does My Device Labeling Comply with 21 CFR 801?
Understanding The Relationship Between Usability and Labeling of Your Medical Device
Get your free Checklist
FDA Labeling Requirements Checklist